Patient and Family Education and Discharge Planning
In the case of a traumatic injury, the perioperative nurse plays a key role in supporting the patient and family.
The nurse may call the surgical waiting room and provide the family with updates on the patient’s progress, after checking with the surgeon on what should be communicated.
Some patients may experience post-traumatic stress disorder and need continued therapy, which may be provided on an outpatient basis. Hospitals may provide access to support groups for patients and families related to the type of injury and its extended effects.
(Gawronski, 2019)
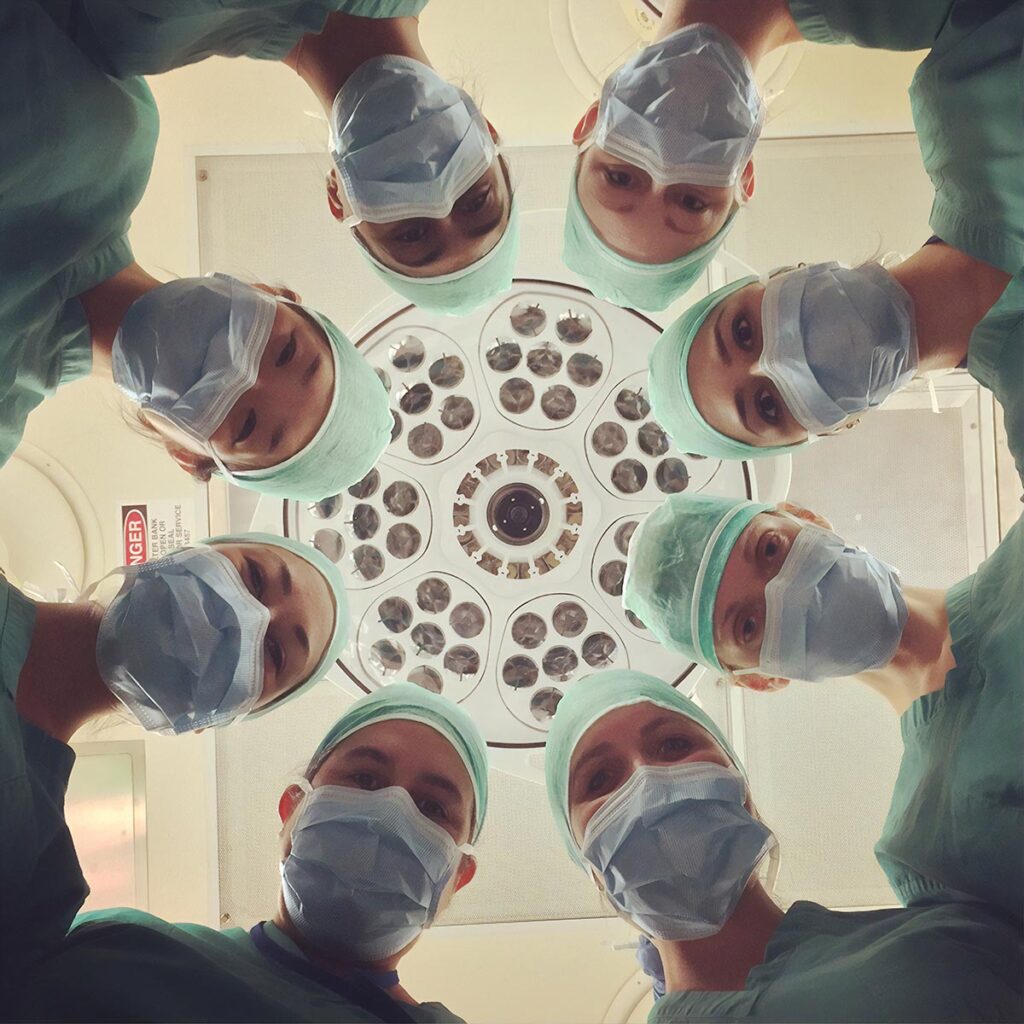
💬 Communication Highlights: Interprofessional Team
Teamwork in the OR setting includes professional interactions with the following:
- Surgeon(s)
- Anaesthesiologist
- Emergency department
- OR nurses
- ICU nurses
- Transfusion lab
(Ross, 2006)
💬 Communication Highlights: Family
- When communicating with the family, nurses must involve the surgeon and anesthesiologist.
- Nurses must find out what has been discussed with the family or what is appropriate to disclose.
- When talking to the family, it is helpful to use plain language.
- To ensure the family understands the information, nurses should get them to repeat what has been said and encourage them to ask questions.
(Gawronski, 2019)
Mass Casualty
Trauma cases often involve more than one victim. Especially with collisions, fires, and natural disasters, it’s likely that more than one patient will be admitted with varying levels of injury. Even if patients are brought to a large trauma centre, there may be challenges with:
- Staffing from any member of the interprofessional team
- Availability of blood
- Availability of supplies such as X-ray, trauma/vascular/emergency surgical equipment
Code Orange
Each hospital should have a code orange protocol. This code is used to respond to an external disaster that has a high likelihood of sending an influx of patients to the facility. The protocol allows areas such as the emergency room, operating room, and intensive care units to ask staff to stay beyond their shifts or to be called in to support increased needs.
Code Orange: Inside The Ottawa Hospital’s response – The Ottawa Hospital
Review this local story to learn more about how the Ottawa Hospital prepared for and managed a code Orange:
Read Article
Operating Room Capacity
The perioperative environment is reliant on staffing from multiple members of the extraprofessional team to support and run additional rooms. If multiple trauma patients arrive in the emergency department requiring surgery, the surgical team must prioritize based on their ability to run additional rooms.
During the day, if there are elective cases, the OR charge nurse, surgeons and anesthesia care providers, will place elective cases on hold to free up rooms and staff for surgery.
In the evenings and nights, additional staff may be called in to support trauma cases. Even with additional staffing, there may be a need to prioritize.
Prioritizing Cases
The OR charge nurse, anesthesia care provider, and surgeon will work together to prioritize the trauma patients requiring surgery. If staffing permits, patients may be brought to the OR concurrently. However, if this is not possible, patients will need to be prioritized using something like this Urgent-Emergent Case Classification system. This is also used to classify urgent non trauma patients.
Urgent-Emergent Case Classification
(OR Manager, 2010)
Graded Activity
In Blackboard, complete the Graded Activity: Prioritizing Case Study
Summary
Communication plays a key role in providing care for trauma patients. Open communication with the emergency department, surgeon and anaesthesiologist will assist with the management of the stressful situation. The OR nurse’s preoperative assessment is significant in how to navigate the preparation for surgery. Knowing and understanding the MOI will assist the OR nurse in the preparation. That will allow the nurse to ask the surgeon and anaesthesiologist pertinent questions related to the procedure set up. Open communication exhibits teamwork and helps the nurse in staying focused and calm.